Ver evolución gráfica del caso
Introduction
After a tooth is lost, a number of dimensional changes will occur in the alveolar bone and, consequently, in the soft tissues, frequently causing defects in the alveolar ridge that can hinder or impede good implant positioning. It can also prevent us from achieving acceptable results from an aesthetic point of view, especially in the anterior sector. Socket preservation.
To prevent and treat these defects, there are different techniques that aim to preserve or increase the hard and/or soft tissues. Slight defects can generally be resolved by augmenting the soft tissues. Nevertheless, in cases with significant bone loss or where the treatment includes implant-supported prostheses, the combination of various techniques at different stages may be necessary. Socket preservation.
Case presentation
Male patient, 51 years of age, with no medical history of interest, consulted the clinic due to a work incident in which he received a strong blow to the upper incisors.
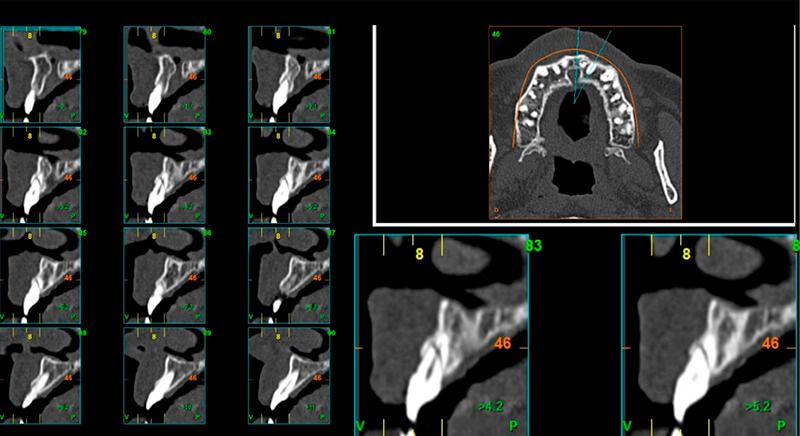
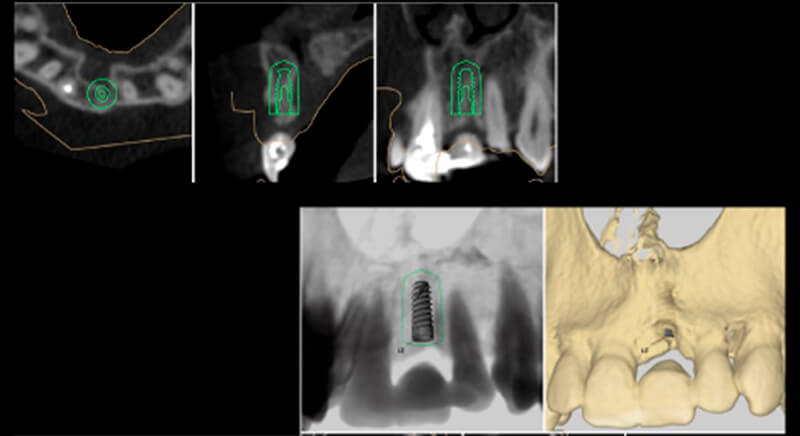
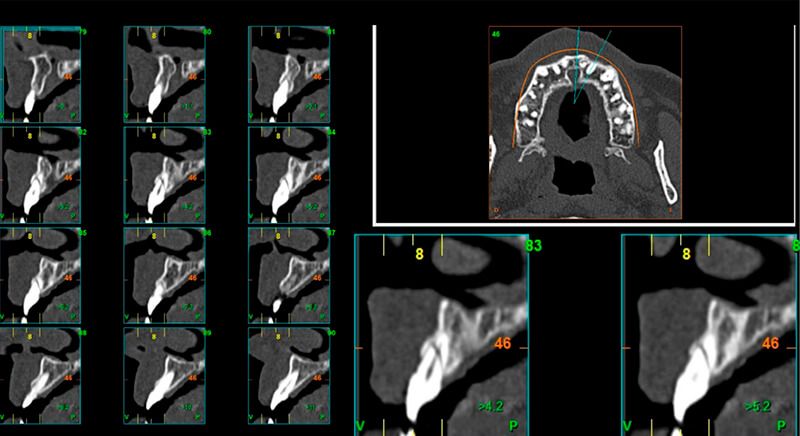
As result of an exhaustive examination a fracture of tooth 1.1 was detected, and although at first a fracture of 2.1 was not observed, it did present movement. Finally, the CT images revealed a radicular apical fracture of tooth 2.1 that meant the tooth could not be saved.


Treatment plan
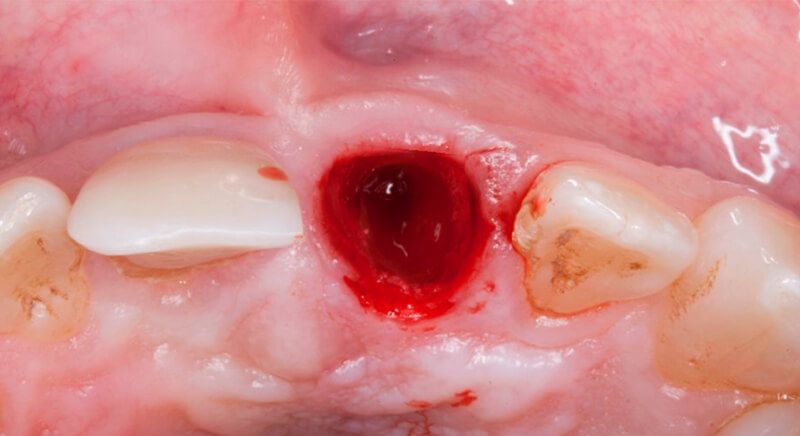
It was decided to reconstruct tooth 1.1 and perform endodontic work up to the fracture line of tooth 2.1 so it could be maintained provisionally, but the patient was very uncomfortable and unable to chew in this area so it was finally decided to extract both the coronal part and the fractured apex of tooth 2.1.



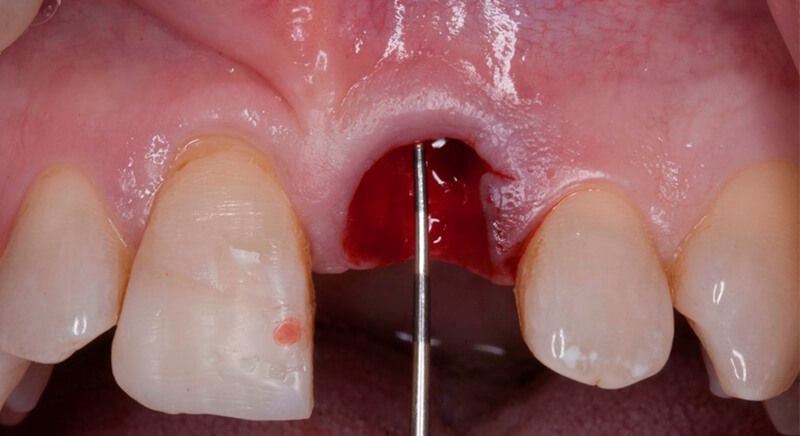

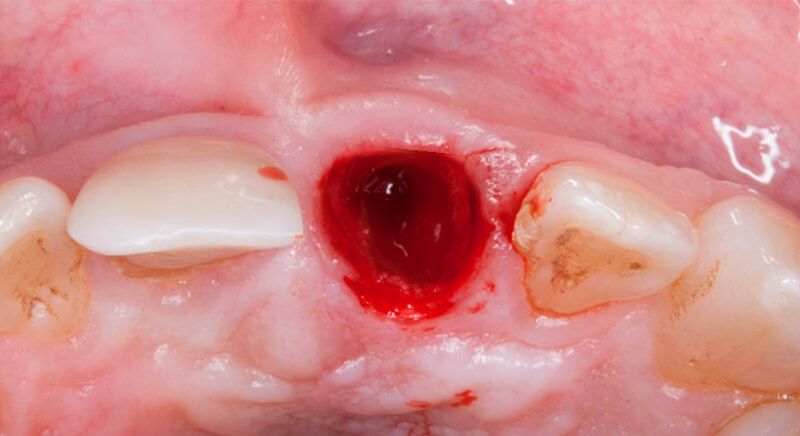
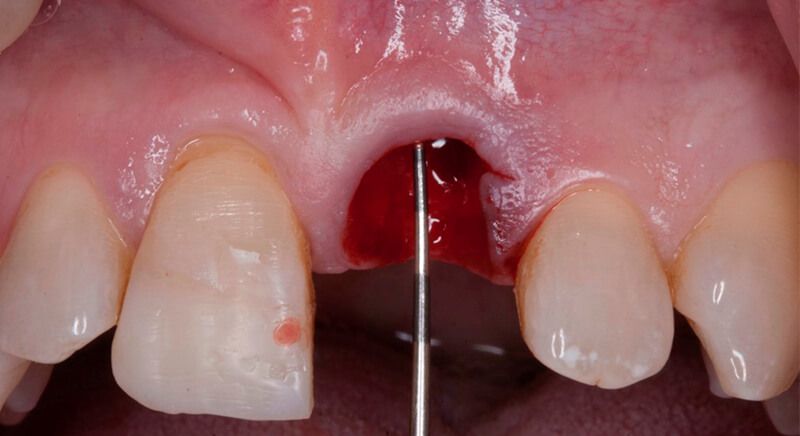
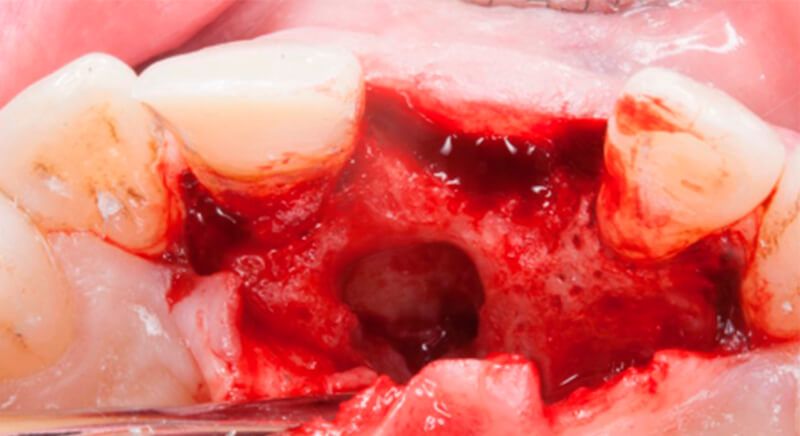
Once tooth 2.1 had been extracted, it was decided that it was not advisable to place an implant immediately as the bone conditions were not ideal and the gum did not have sufficient thickness. We opted for a treatment to preserve the socket and to delay implant insertion.
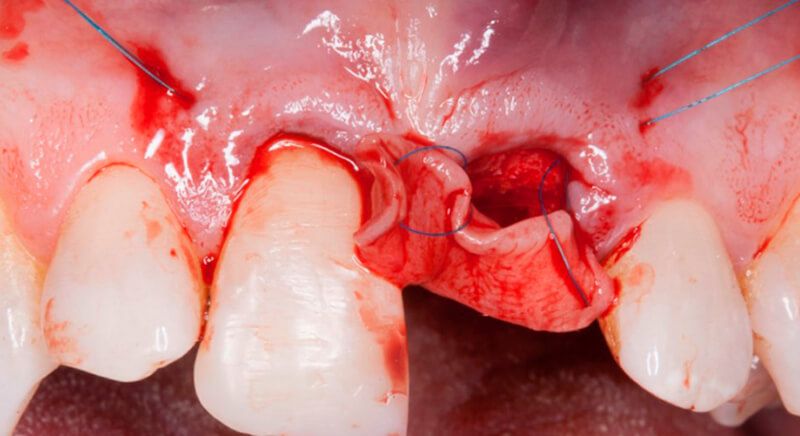
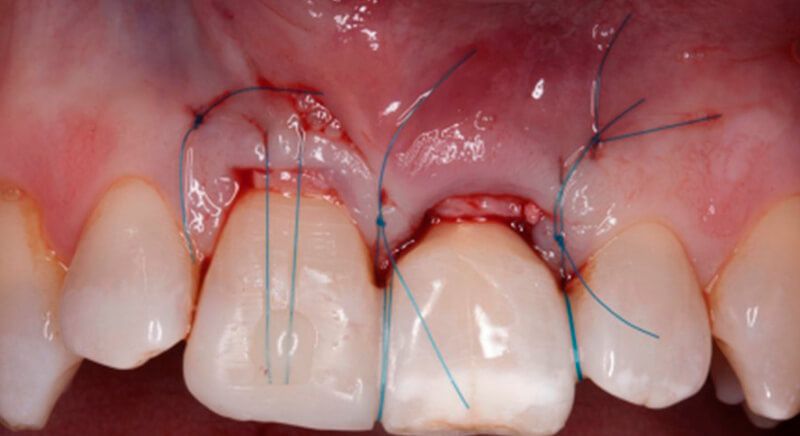
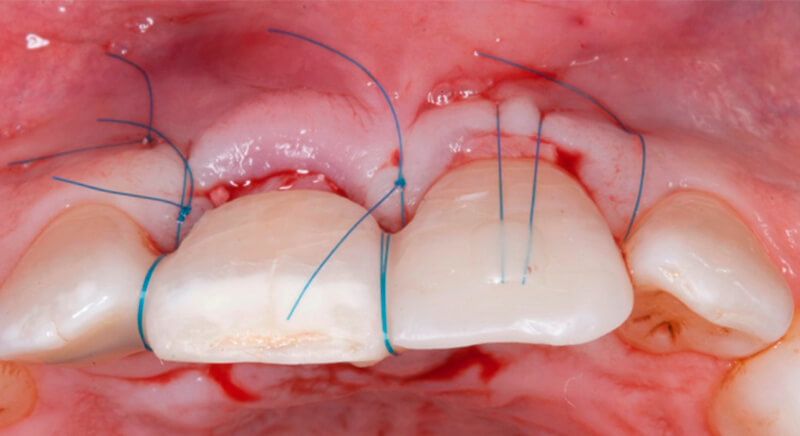
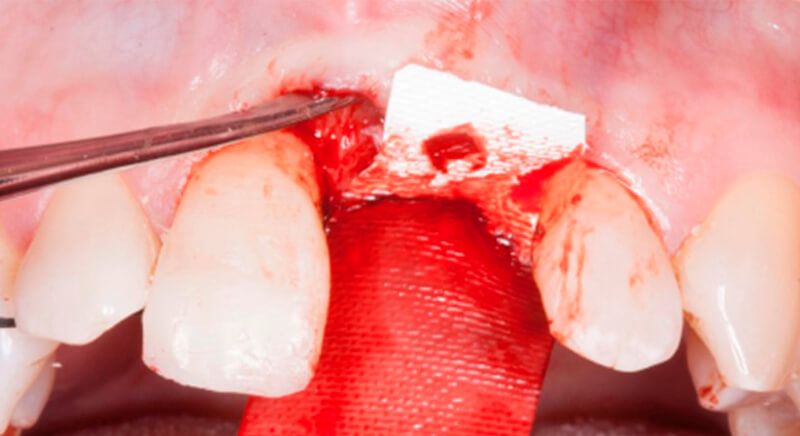
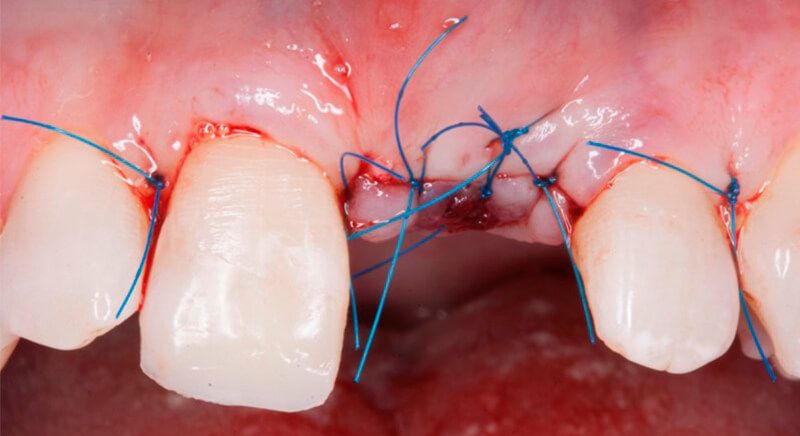
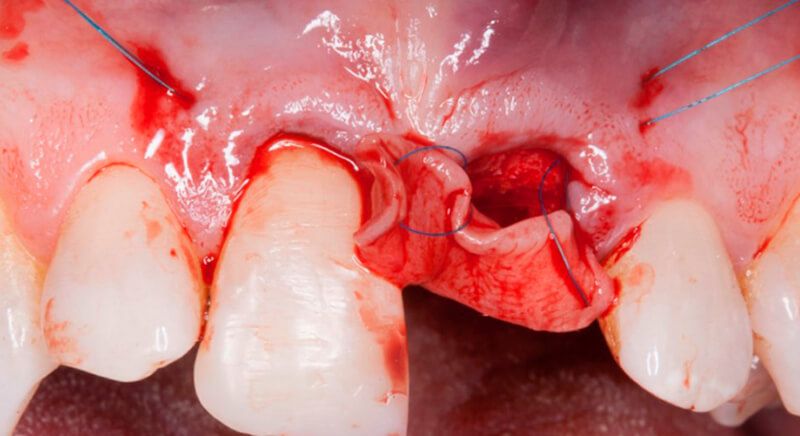
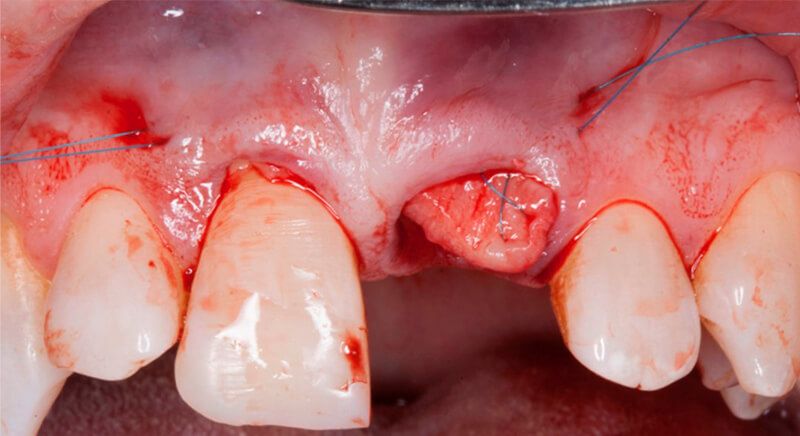
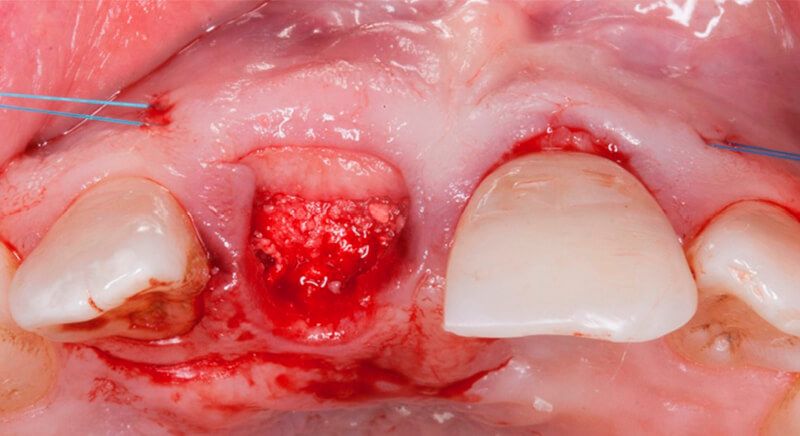
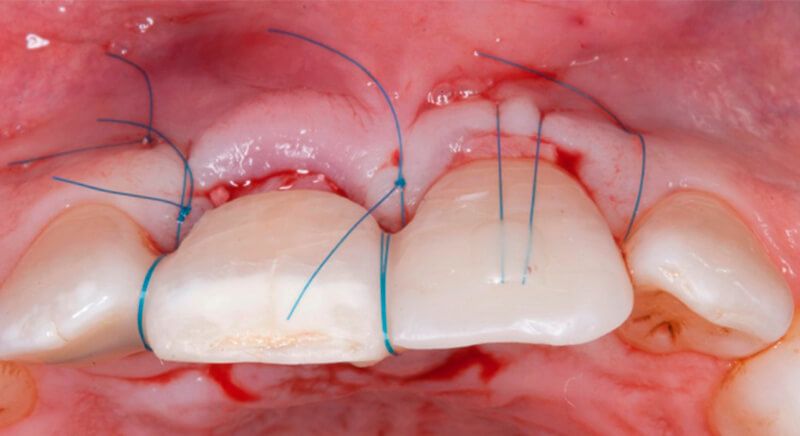
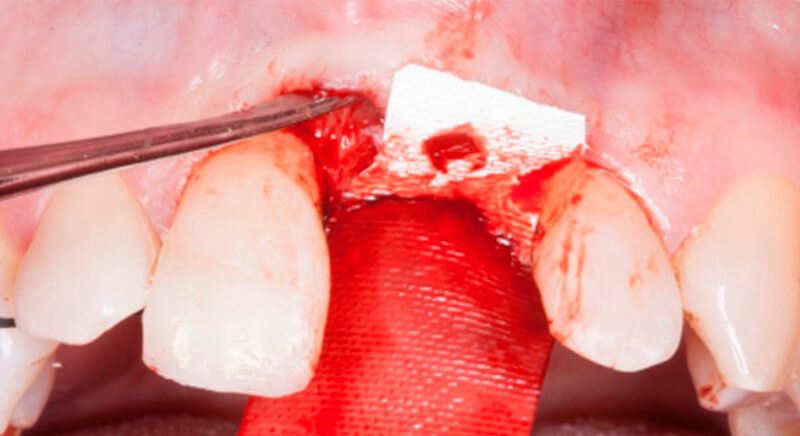
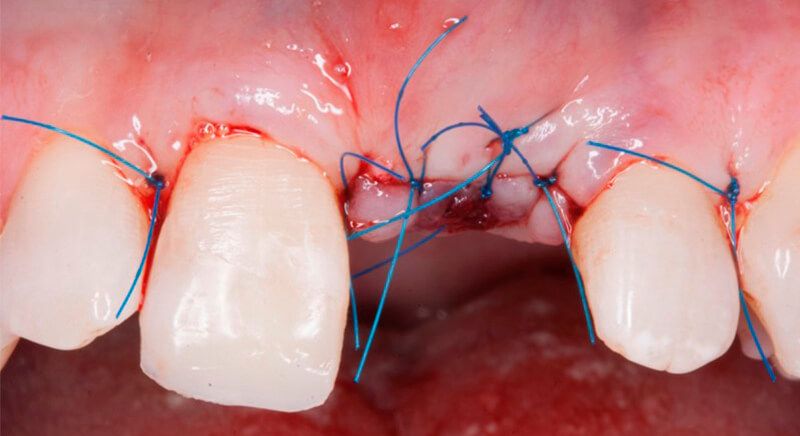
The socket was filled with a xenograft after the extraction and a graft of connective tissue was placed in the vestibular area of the two upper central incisors.
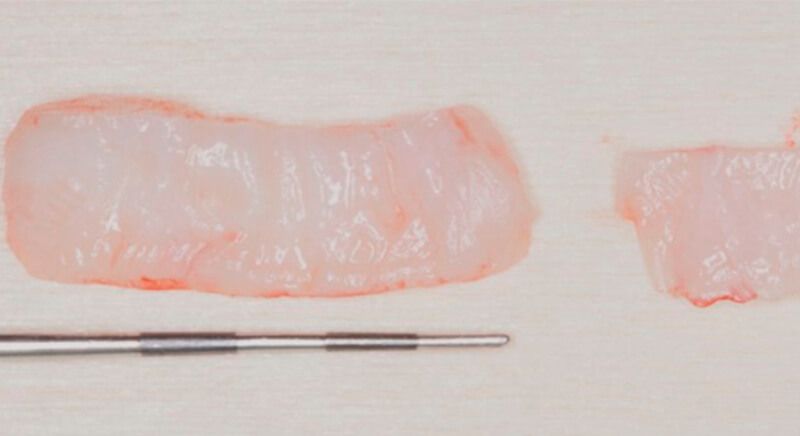
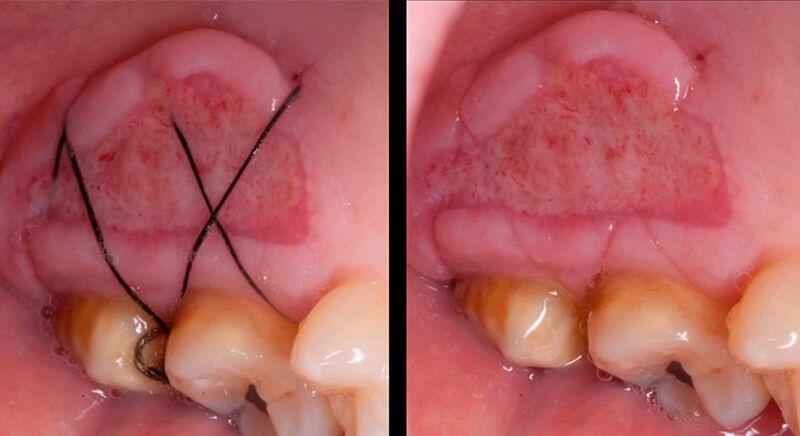
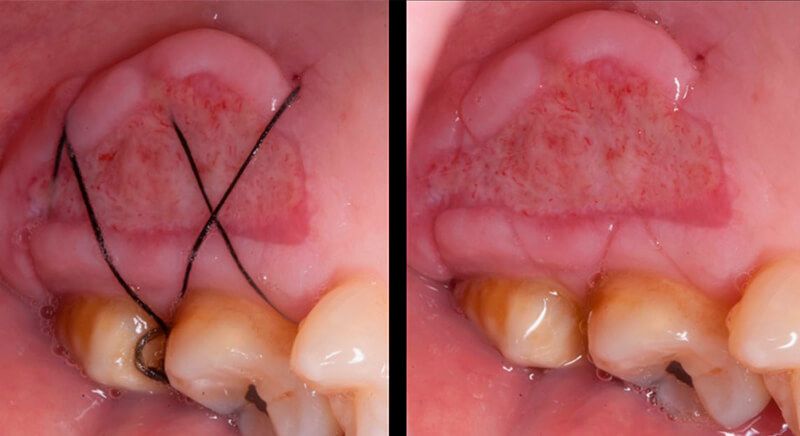
The tissue with epithelium was taken from the palate and de-epithelialized outside of the mouth. This obtains a lamina propria graft with better density and quality than if it were obtained with a single incision to the palate.


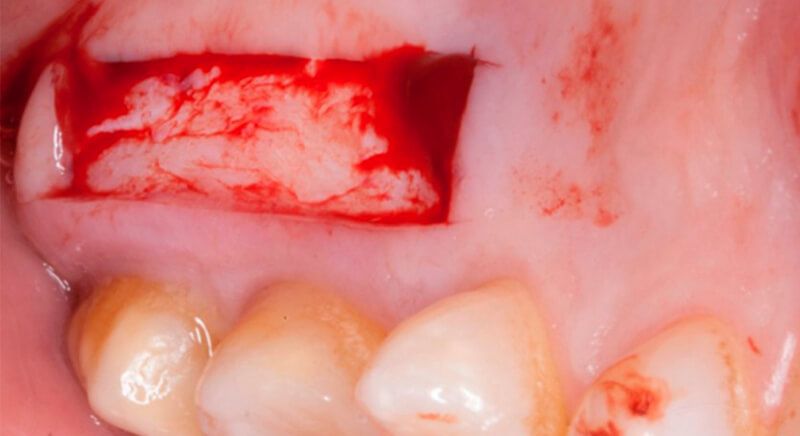




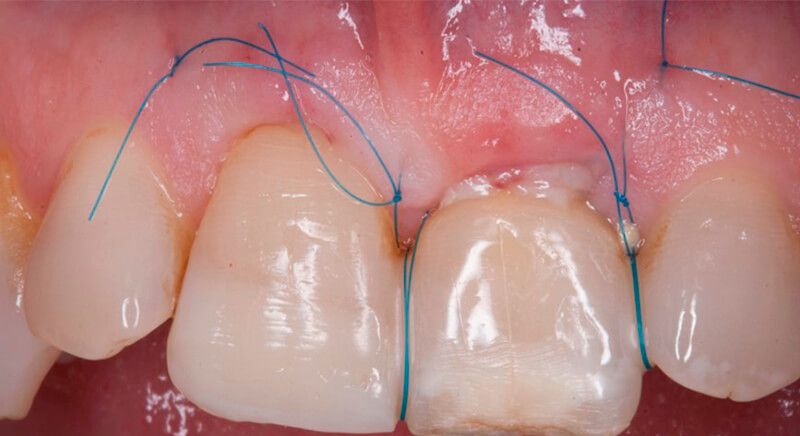

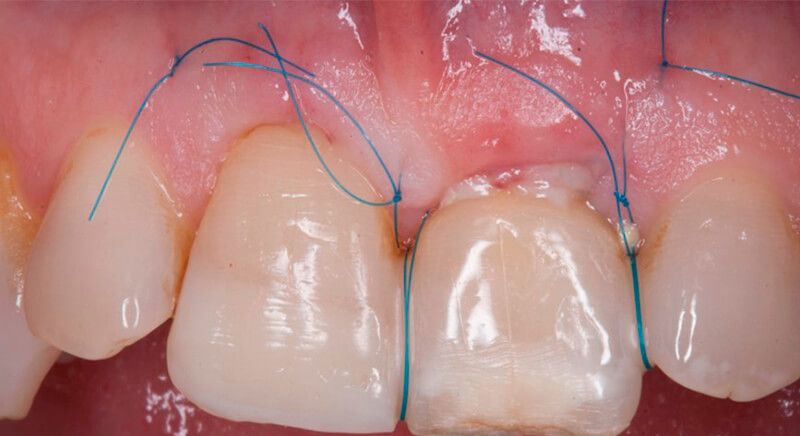
Once the hard and soft tissues had healed, 6 months after the surgery, a good volume remained in the vestibular area. It was then that we could consider an implant, using guided surgery to ensure it was placed in the correct three-dimensional position.




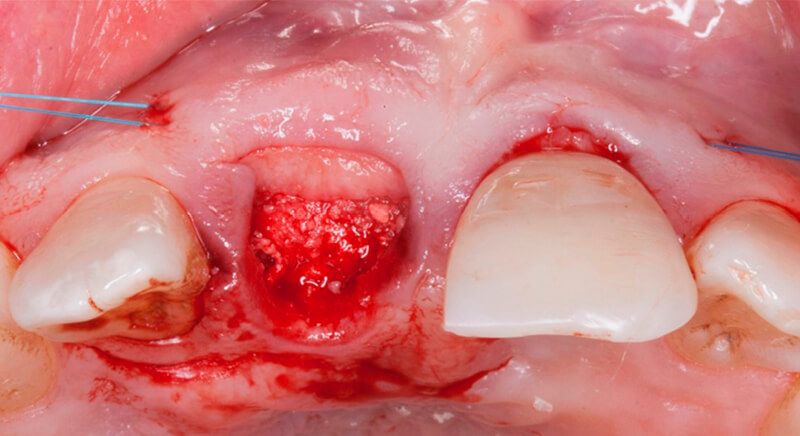
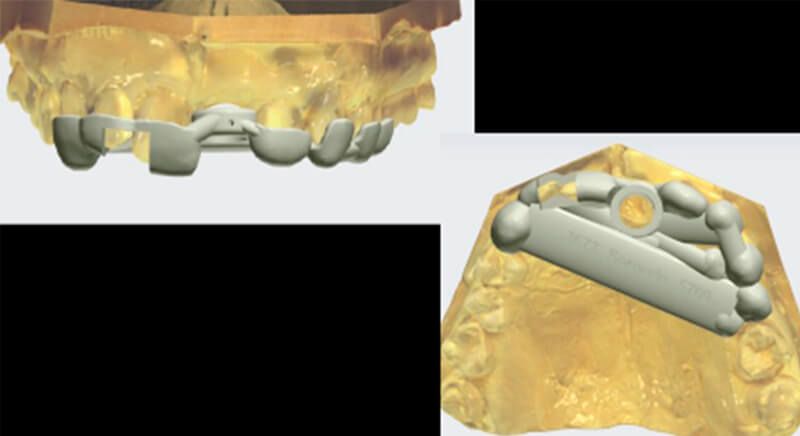
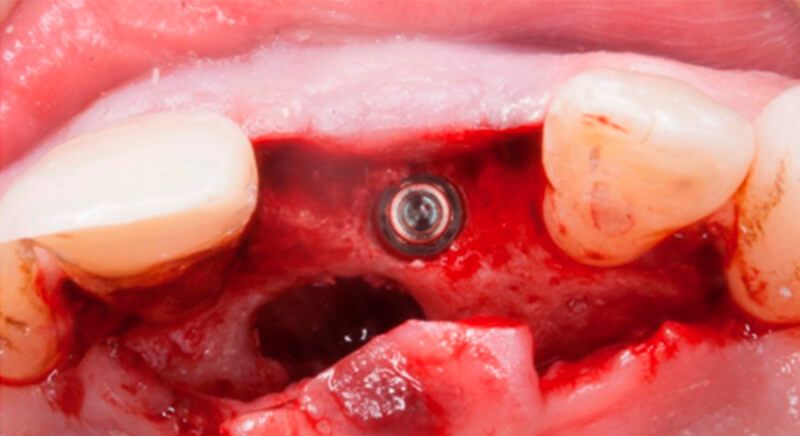
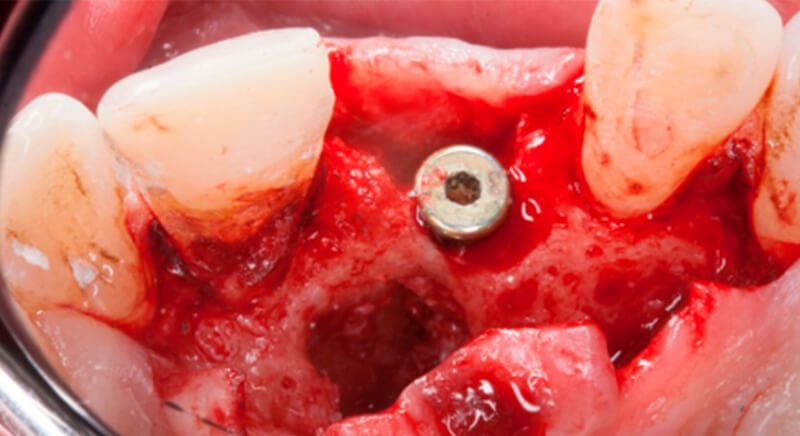
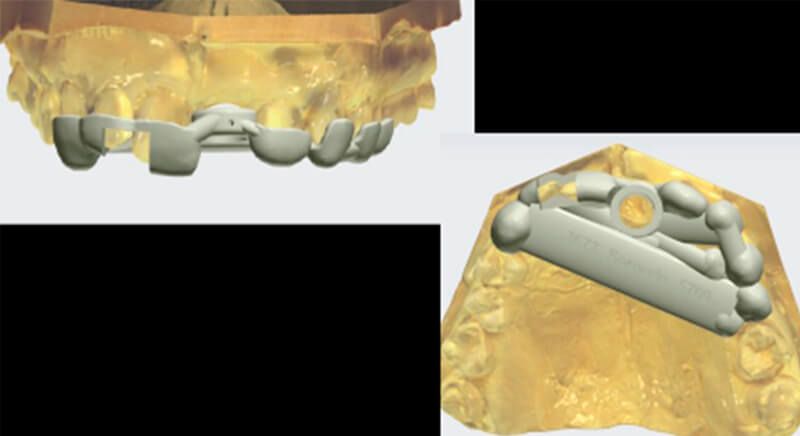
During the digital planning for the implant, with Implant Studio (3Shape) guided surgery software, significant bone defects due to the patient's anatomy were discovered. Placing the implant in the correct position for the prosthesis presented bone dehiscence in the vestibular area, and another bone defect in the palatine area due to the patient's large nasopalatine canal.
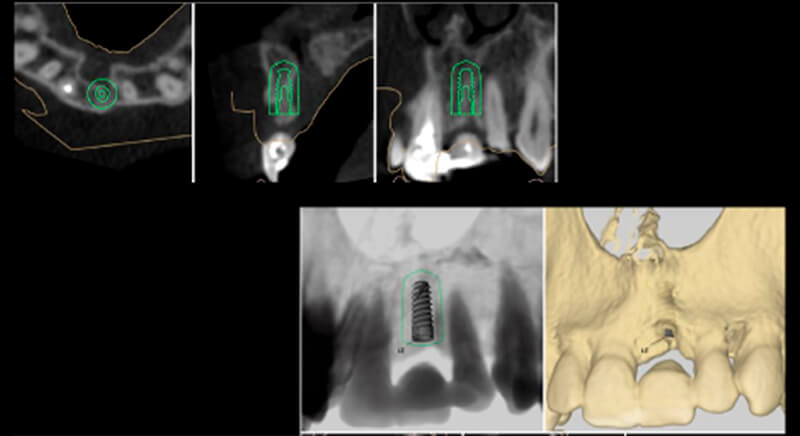
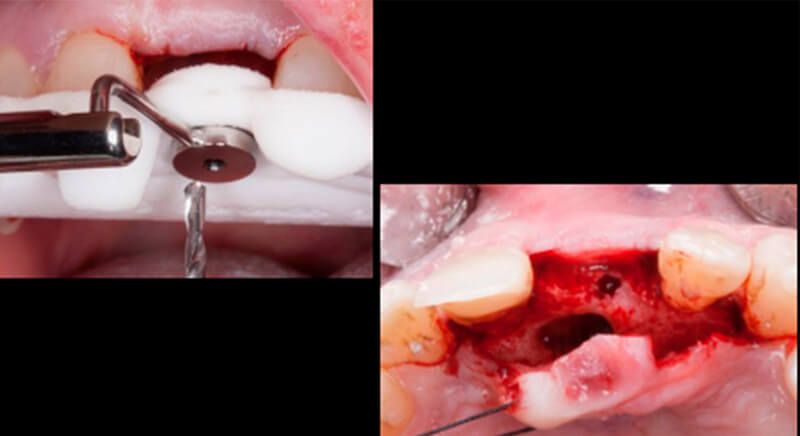
This information enabled us to rule out the option of surgery without a flap, as regeneration simultaneous to surgery would be needed, so the idea of using guided surgery was maintained.
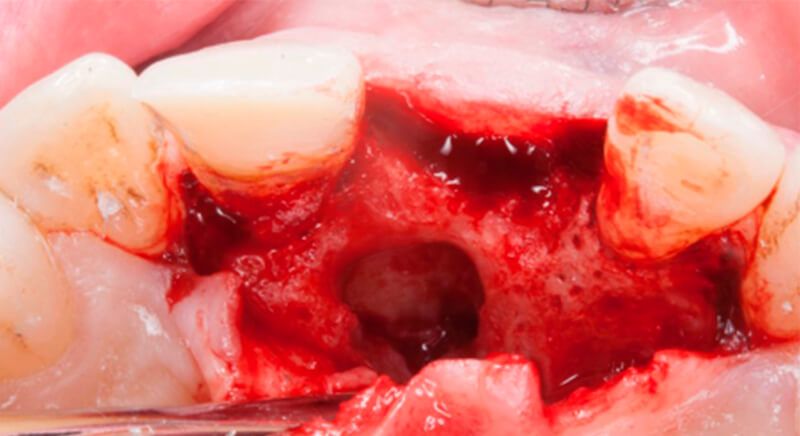

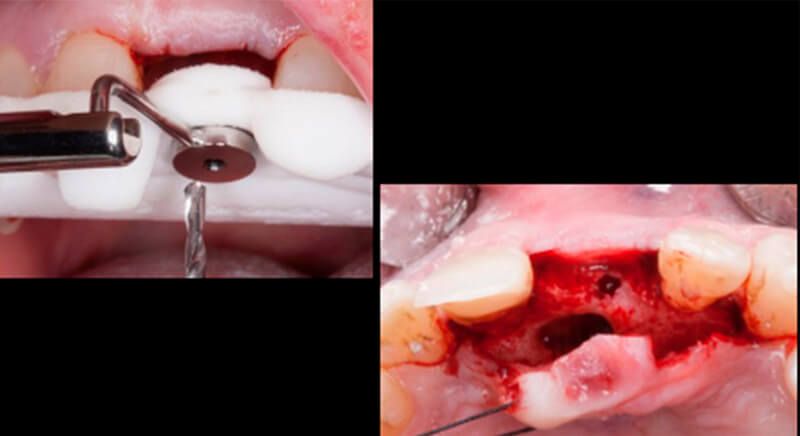
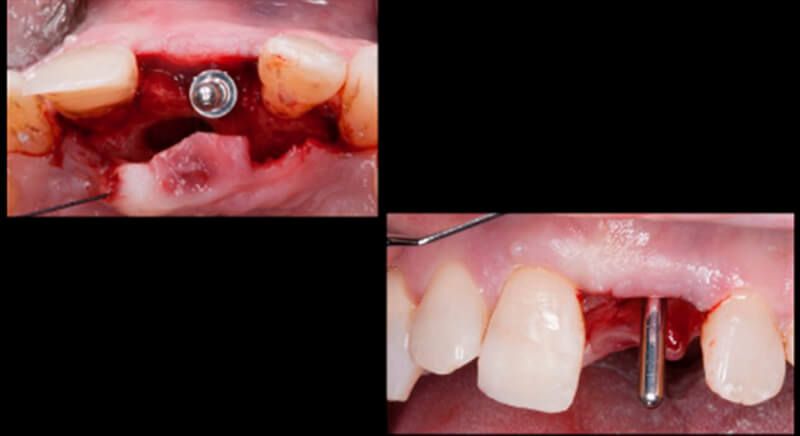
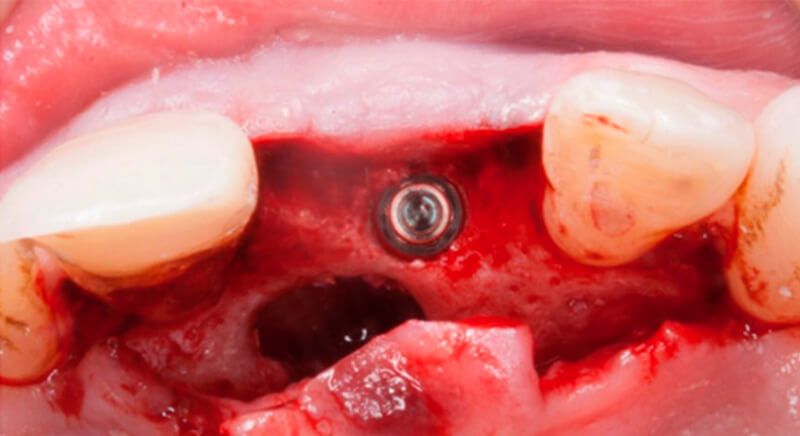
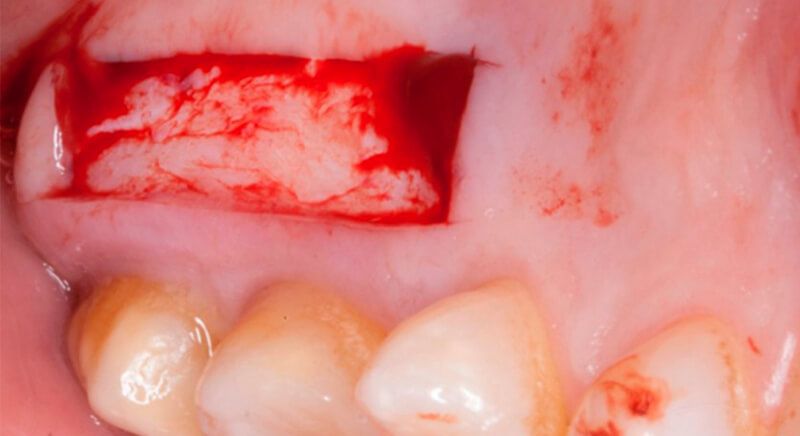
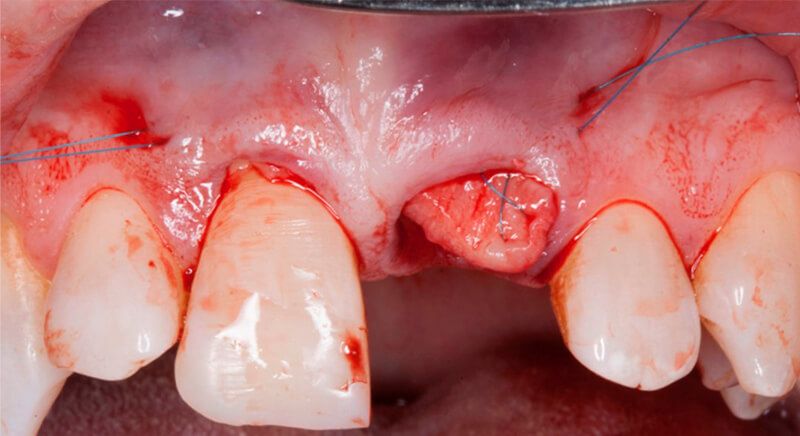
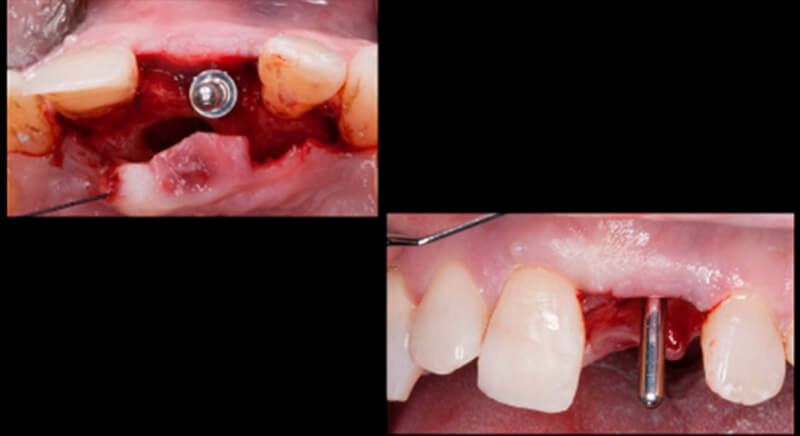
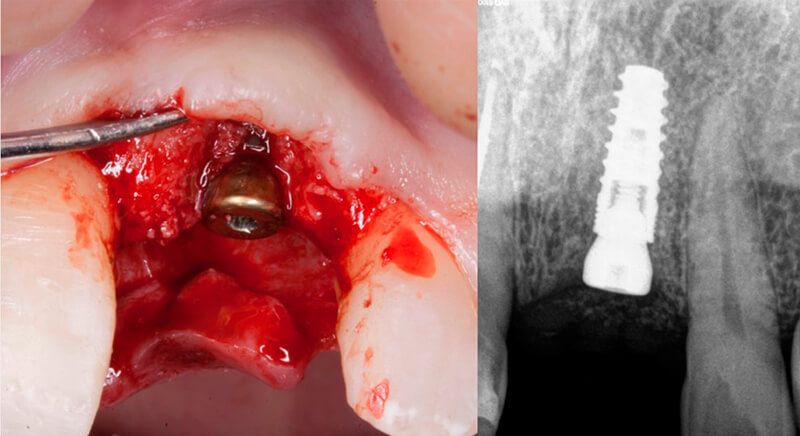
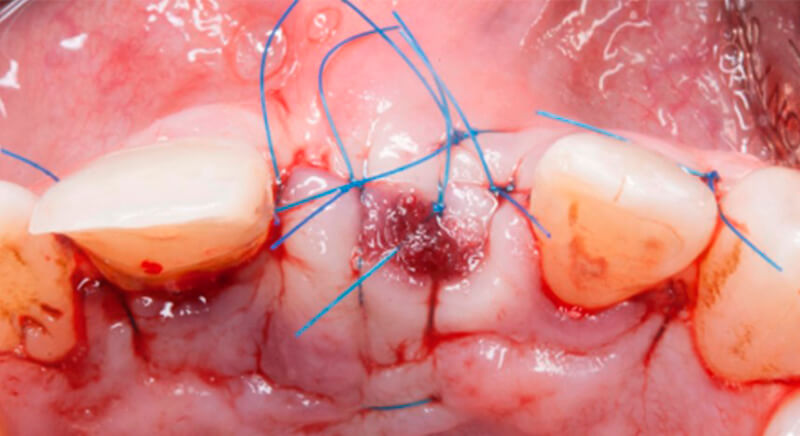
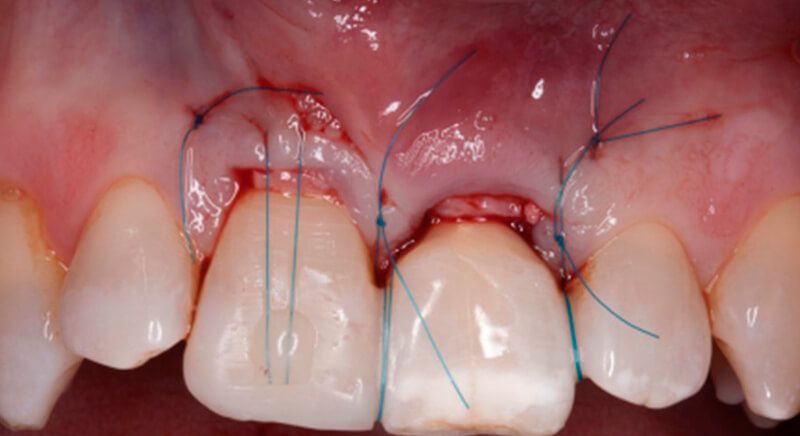
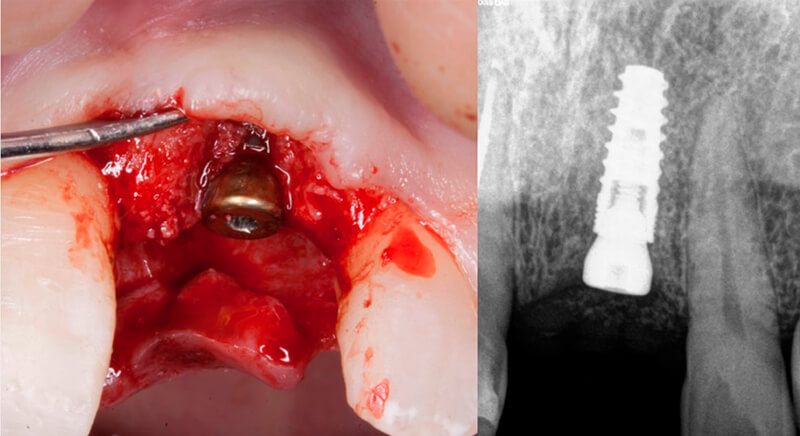
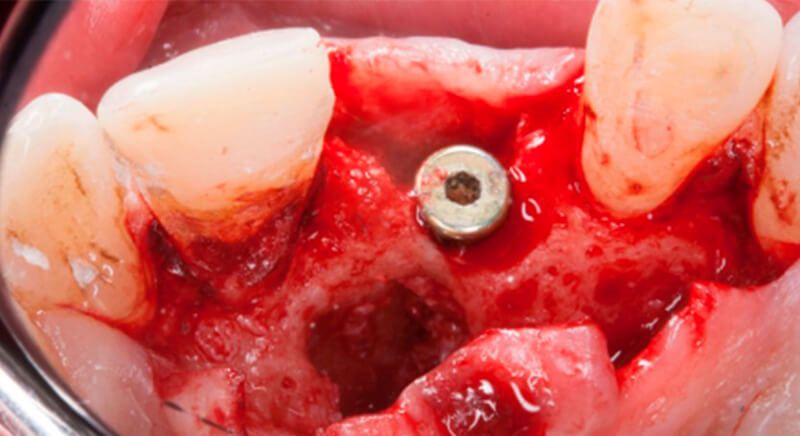
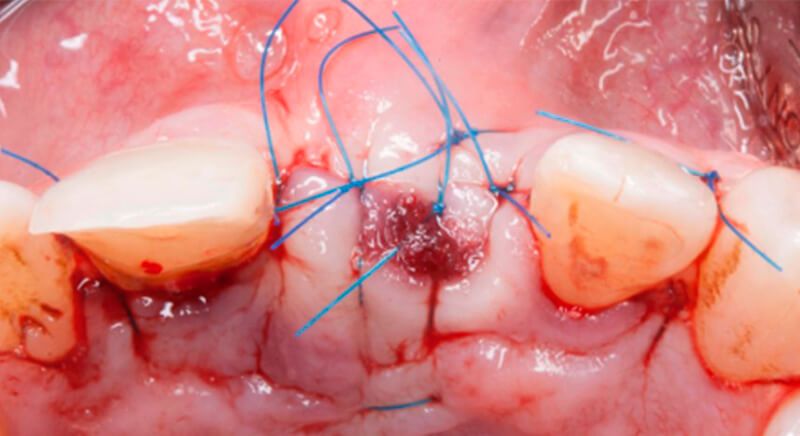
The guided surgery was performed by lifting a full thickness mucoperiosteal flap. A Biomimetic Ocean CC implant, diameter 3.5mm and length 10mm, was inserted using the surgical guide in the ideal three-dimensional position and the defects were regenerated with xenograft and reabsorbable membrane, the nasopalatine duct on the palatine side and the area of dehiscence on the vestibular.
During the same surgical intervention, a short 3mm Avinent healing abutment was positioned and fully covered by the flap. Primary closure was completed and we waited 6 months for the bone graft to mature.






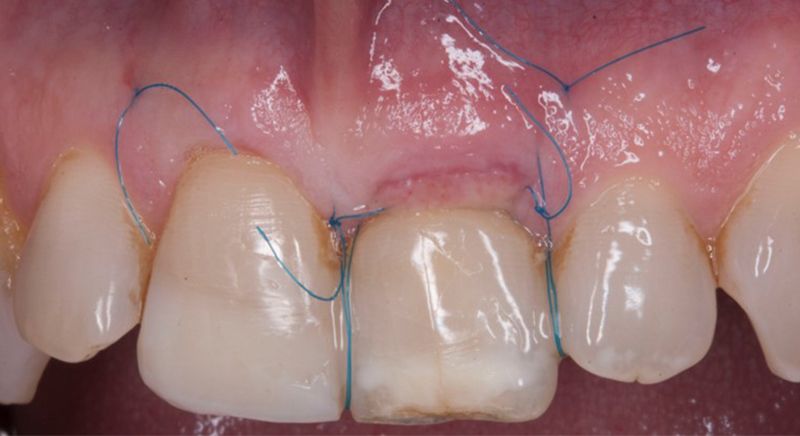
After 6 months of healing, a minimum crestal incision was made to change the 3mm abutment underneath for a 5mm abutment that would be exposed to the oral medium.

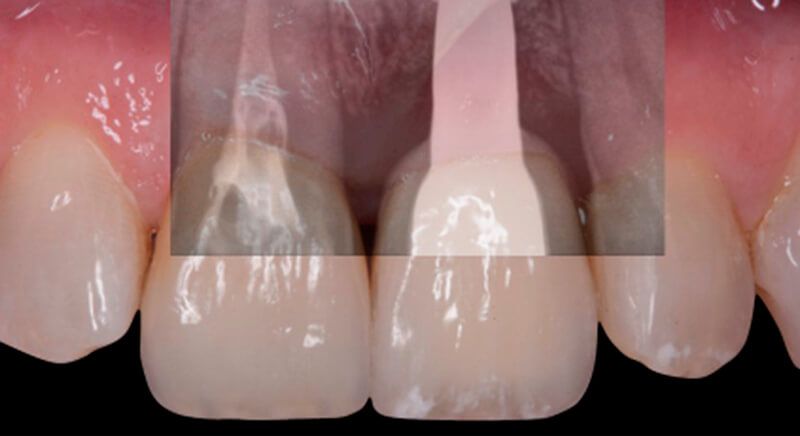
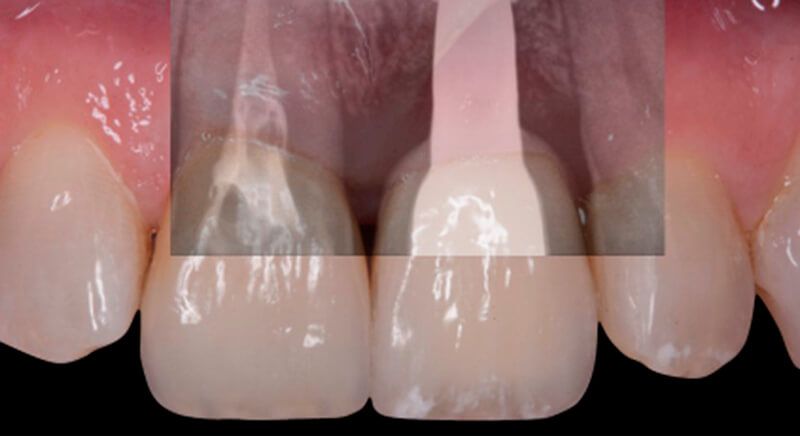
Finally, a definitive metal ceramic crown was designed and manufactured for 2.1 and a veneer for 1.1.




Conclusions
Tooth loss can cause dimensional changes to both hard and soft tissues that affect the patient's final appearance, above all with treatments in the anterior sector.
If the treatment also includes dental implants, a correct diagnosis of the defect, good planning of the three-dimensional position of the implants, selection of the surgical technique and treatment of the soft tissues during the provisional restoration are important for predictable aesthetic results.
This clinical case shows the anticipation of the changes in volume that are going to occur after the dental extraction in terms of both bone and soft tissues.
Moreover, guided surgery makes it possible to place the implant in the correct three-dimensional position, despite unfavourable bone anatomy.